MultiHance®
(gadobenate dimeglumine)
MultiHance® (gadobenate dimeglumine) is a gadolinium-based contrast agent (GBCA) currently approved in the European Union, Norway and Iceland for use in diagnostic magnetic resonance imaging (MRI) of the liver in adult and in pediatric patients older than two years of age.1
The active ingredient of MultiHance® (gadobenate dimeglumine, or Gd-BOPTA) possesses an aromatic (benzyloxymethyl) group on the contrast-effective molecule.
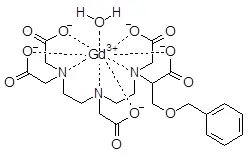
Thanks to its chemical structure, Gd-BOPTA is actively transported into functioning hepatocytes and up to 4% of the injected dose is excreted via the hepatobiliary route into the bile and, ultimately, the faeces.2, 3, 4
In view of its pharmacokinetics, MultiHance® can be used both for dynamic and delayed, liver-specific imaging in adult and pediatric patients.
Evidence shows that:
- Dynamic imaging is not affected by short-term dyspnea and respiratory motion artifacts 5, 6, 7
- Delayed, liver-specific imaging offers extended opportunities for the assessment of focal liver lesions, with further increase in sensitivity and specificity for detection and characterization of liver disease over and above those provided by dynamic imaging when images are acquired 40-120 minutes after injection of the agent. 8, 9, 10, 11
Therefore, MultiHance® should be used when diagnostic information is essential and not available with unenhanced MRI and when delayed phase imaging is required.
The aromatic group on Gd-BOPTA also provides increased r1-relaxivity relative to that of the macrocyclic GBCAs12, 13, 14, 15 and hence greater signal intensity (SI) enhancement on T1-weighted images16. This is why MultiHance allows both dynamic and delayed, organ-specific imaging of the liver at a dose as low as 0.05 mmol/kg.
Therefore, the recommended dose of MultiHance in adult patients and children is 0.05 mmol/kg body weight (0.1 mL/kg of the 0.5 M solution). The lowest dose that provides sufficient enhancement for diagnostic purposes should be used. The dose should be calculated based on the patient's body weight, and should not exceed the recommended dose per kilogram of body weight.1
The safety of MultiHance has been established in numerous clinical investigations and during extensive clinical use with 35 million doses administered worldwide since its launch.17, 18, 19, 20
The safety of MultiHance has also been studied in children and in special populations, such as children and patients with impairment of renal and/or liver function. 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32
1) MultiHance Summary of Product Characteristics
2) Gadobenate dimeglumine (Gd-BOPTA). An overview
Kirchin MA, Pirovano GP, Spinazzi A. Invest Radiol 1998; 33: 798–809
3) Safety, tolerance, biodistribution and MR imaging enhancement of the liver with gadobenate dimeglumine: results of clinical pharmacologic and pilot imaging studies in nonpatient and patient volunteers
Spinazzi A, Lorusso V, Pirovano GP, Kirchin M. Acad Radiol 1999; 6: 282–91
4) Hepatobiliary MR imaging with gadolinium-based contrast agents
Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, et al. J Magn Reson Imaging 2012; 35: 492-511.
5) Matched within-patient cohort study of transient arterial phase respiratory motion-related artifact in MR imaging of the liver: gadoxetate disodium versus gadobenate dimeglumine
Davenport MS, Caoili EM, Kaza RK, Hussain HK. Radiology 2014; 272:123-31
6) Transient arterial phase respiratory motion-related artifact in MR imaging of the liver: an analysis of four different gadolinium-based contrast agent
Shah MR, Flusberg M, Paroder V, Rozenblit AM, Chernyak V. Clin Imaging 2017; 41: 23-27.
7) Effect of Gadoxetate Disodium on Arterial Phase Respiratory Waveforms Using a Quantitative Fast Fourier Transformation-Based Analysis
Davenport MS, Malyarenko DI, Pang Y, Hussain HK, Chenevert TL. AJR Am J Roentgenol. 2016 Dec 8:W1-W9. [Epub ahead of print]
8) Gadobenate dimeglumine-enhanced liver MR imaging: value of dynamic and delayed imaging for the characterization and detection of focal liver lesions
Kim YK, Lee JM, Kim CS. Eur Radiol 2004;14: 5-13.
9) Hepatocellular carcinoma in patients with cirrhosis: qualitative comparison of gadobenate dimeglumine-enhanced MR imaging and multiphasic 64-section CT
Marin D, Di Martino M, Guerrisi A, De Filippis G, Rossi M, Ginanni Corradini S, et al. Radiology 2009; 251: 85-95.
10) Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study
Grazioli L, Morana G, Kirchin MA, Schneider G. Radiology 2005; 236: 166-77.
11) Solid hypervascular liver lesions: accurate identification of true benign lesions on enhanced dynamic and hepatobiliary phase magnetic resonance imaging after gadobenate dimeglumine administration
Morana G, Grazioli L, Kirchin MA, Bondioni MP, Faccioli N, Guarise A, Schneider G. Invest Radiol 2011; 46: 225-39.
12) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths
Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ. Invest Radiol 2005; 40: 715-24
13) Comparative study of the physicochemical properties of six clinical low molecular weight gadolinium contrast agents
Laurent S, Vander Elst L, Muller RN. Contrast Med Mol Imaging 2006;1:128–37
14) Influence of human serum albumin on longitudinal and transverse relaxation rates (r1 and r2) of magnetic resonance contrast agents
Giesel FL, von Tengg-Kobligk H, Wilkinson ID, Siegler P, von der Lieth CW, Frank M, et al. Invest Radiol 2006;41:222-28
15) T1 relaxivities of gadolinium-based magnetic resonance contrast agents in human whole blood at 1.5, 3, and 7 T
Shen Y, Goerner FL, Snyder C, Morelli JN, Hao D, Hu D, Li X, Runge VM. Invest Radiol. 2015 May;50(5):330-8
16) A serial dilution study of gadolinium-based MR imaging contrast agents
Bleicher AG, Kanal E. AJNR Am J Neuroradiol 2008; 29: 668-73
17) Assessment of rates of acute adverse reactions to gadobenate dimeglumine: review of more than 130,000 administrations in 7.5 years
Fakhran S, Alhilali L, Kale H, Kanal E. AJR Am J Roentgenol 2015; 204:703-6
18) A. Safety characteristics of gadobenate dimeglumine: clinical experience from intra- and interindividual comparison studies with gadopentetate dimeglumine
Shellock FG, Parker JR, Pirovano G, Shen N, Venetianer C, Kirchin MA, Spinazzi J Magn Reson Imaging 2006; 24:1378-85
19) Safety of gadobenate dimeglumine (MultiHance): Summary of findings from clinical studies and postmarketing surveillance
Shellock FG, Parker JR, Venetianer C, Pirovano G, Spinazzi A. Invest Radiol 2006; 41: 500-9
20) Bracco Data on File
21) Safety and adverse effects during 24 hours after contrast-enhanced MRI with gadobenate dimeglumine (MultiHance) in children
Schneider G, Schürholz H, Kirchin MA, Bücker A, Fries P. Pediatr Radiol 2013; 3:202-11
22) Renal safety of intravenous gadolinium-enhanced magnetic resonance imaging in patients awaiting liver transplantation
Shaffer KM, Parikh MR, Runge TM, Perez SD, Sakaria SS, Subramanian RM. Liver Transpl. 2015 Nov;21(11):1340-6
23) Advancing pharmacovigilance through academic-legal collaboration: the case of gadolinium-based contrast agents and nephrogenic systemic fibrosis-a Research on Adverse Drug Events and Reports (RADAR) report
Edwards BJ, Laumann AE, Nardone B, Miller FH, Restaino J, Raisch DW, McKoy JM, Hammel JA, Bhatt K, Bauer K, Samaras AT, Fisher MJ, Bull C, Saddleton E, Belknap SM, Thomsen HS, Kanal E, Cowper SE, Abu Alfa AK, West DP. Br J Radiol 2014; 87(1042):20140307. doi: 10.1259/bjr.20140307
24) Prospective Cohort Study of Nephrogenic Systemic Fibrosis in Patients With Stage 3-5 Chronic Kidney Disease Undergoing MRI With Injected Gadobenate Dimeglumine or Gadoteridol
Soulez G, Bloomgarden DC, Rofsky NM, Smith MP, Abujudeh HH, Morgan DE, Lichtenstein RJ, Wippold FJ 2nd, Russo C, Kuhn MJ, Mennitt KW, Maki JH, Stolpen A, Liou J, Semelka RC, Kirchin MA, Shen N, Pirovano G, Spinazzi A. AJR Am J Roentgenol 2015; 205:469-78
25) Evaluation of the incidence of nephrogenic systemic fibrosis in patients with moderate renal insufficiency administered gadobenate dimeglumine for MRI
Bryant BJ, Im K, Broome DR. Clin Radiol 2009;64:706-13.
26) Retrospective assessment of prevalence of nephrogenic systemic fibrosis (NSF) after implementation of a new guideline for the use of gadobenate dimeglumine as a sole contrast agent for magnetic resonance examination in renally impaired patients
Abujudeh HH, Rolls H, Kaewlai R, Agarwal S, Gebreananya ZA, Saini S, et al. J Magn Reson Imaging 2009;30:1335-40.
27) Nephrogenic systemic fibrosis: change in incidence following a switch in gadolinium agents and adoption of a gadolinium policy--report from two U.S. universities
Altun E, Martin DR, Wertman R, Lugo-Somolinos A, Fuller ER 3rd, Semelka RC. Radiology 2009;253:689-96.
28) Decreased incidence of NSF in patients on dialysis after changing gadolinium contrast-enhanced MRI protocols
Martin DR, Krishnamoorthy SK, Kalb B, Salman KN, Sharma P, Carew JD, et al. J Magn Reson Imaging 2010;31:440-46.
29) Incidence of nephrogenic systemic fibrosis after adoption of restrictive gadolinium-based contrast agent guidelines
Wang Y, Alkasab TK, Narin O, Nazarian RM, Kaewlai R, Kay J, Abujudeh HH. Radiology. 2011;260:105-11.
30) Prospective cohort study of NSF in patients with stage 3-5 CKD undergoing MRI with gadobenate or gadoteridol
Soulez G, Bloomgarden DC, Rofsky NM, Smith MP, Abujudeh HH, Morgan DE, et al. AJR Am J Roentgenol. 2015;205: 469-78.
31) Gadobenate dimeglumine administration and nephrogenic systemic fibrosis: Is there a real risk in patients with impaired renal function?
Nandwana SB, Moreno CC, Osipow MT, Sekhar A, Cox KL. Radiology 2015;276:741-47.
32) Incidence of nephrogenic systemic fibrosis using gadobenate dimeglumine in 1423 patients with renal insufficiency compared with gadodiamide
Bruce R, Wentland AL, Haemel AK, Garrett RW, Sadowski DR, Djamali A, Sadowski EA. Invest Radiol 2016 Feb 16. [Epub ahead of print].
Contact us
Please fill out the form below and we will get back to you.
DISCLAIMER
For any product or type of product, whether a drug or device, referenced in this website, physicians should carefully review the product's package insert, instructions for use, or user manual prior to patient administration to ensure proper utilization of the product. The local Summaries of Product Characteristics of the main Bracco Imaging products are available on line.
Gadolinium retention
After administration of gadobenic acid, gadolinium can be retained in the brain and in other tissues of the body (bones, liver, kidneys, skin) and can cause dose-dependent increases in T1-weighted signal intensity in the brain, particularly in the dentate nucleus, globus pallidus, and thalamus. Clinical consequences are unknown. The possible diagnostic advantages of using MultiHance in patients who will require repeated scans should be weighed against the potential for deposition of gadolinium in the brain and other tissues.
Impaired renal function
Prior to administration of MultiHance, it is recommended that all patients are screened for renal dysfunction by obtaining laboratory tests. There have been reports of nephrogenic systemic fibrosis (NSF) associated with use of some gadolinium containing contrast agents in patients with acute or chronic severe renal impairment (GFR<30ml/min/1.73m2).
Patients undergoing liver transplantation are at particular risk since the incidence of acute renal failure is high in this group. As there is a possibility that NSF may occur with MultiHance, it should therefore be avoided in patients with severe renal impairment and in patients in the perioperative liver transplantation period unless the diagnostic information is essential and not available with non-contrast enhanced MRI.
Haemodialysis shortly after MultiHance administration may be useful at removing MultiHance from the body. There is no evidence to support the initiation of haemodialysis for prevention or treatment of NSF in patients not already undergoing haemodialysis.
Elderly
As the renal clearance of gadobenate dimeglumine may be impaired in the elderly, it is particularly important to screen patients aged 65 years and older for renal dysfunction.